White papers

Use our white paper search or select a quick entry below to display white papers based on product type, supplier or application.
The 10 latest white papers
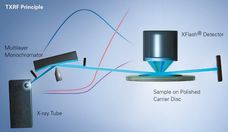
The method of total reflection X-ray fluorescence (TXRF) analysis
How does TXRF work?
View white paper
Spotlight on protein determination: Kjeldahl vs. Dumas
Comparison of the two standard methods for nitrogen and protein determination
View white paper
What are All-Solid-State Batteries
View white paperWhite papers by application
White papers by product type
Promote your white papers on chemeurope.com

You spend a lot of time writing white papers and technical articles and offer them on your website. But the access figures are sobering. What can you do to make your white papers reach more interested parties?
On chemeurope.com, which has over 2.3 million users, your potential customers search specifically for white papers and technical articles that explain methods and explain applications.
You receive high-quality sales leads
You position your company as an expert in your field of expertise
Once written, your content generates sales leads again and again
Curious? Learn more now